- Protein Dictionary.com
- Elia M et al, 2007, Energy values of macronutrients and specific carbohydrates in foods European Journal of Clinical Nutrition
- Calculation of the energy content of foods – energy conversion factors Food and Agriculture Organization
- Dietary Reference intakes: Macronutrients Institute Of Medicine
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) (2005) / 10 Protein and Amino Acids The National Academic Press
- List of foods high in protein US Department of Agriculture
- Typical nutritional composition of mycoprotein Mycoprotein.org
- Proteinuria ─ causes DiagnosisPro
- Martin WF et al, 2005, Dietary protein intake and renal function Nutrition&Metabolism
- Lepe M et al, 2011, Long-term efficacy of high-protein diets: a systematic review SCIELO
- Santesso N et al, 2012, Effects of higher- versus lower-protein diets on health outcomes: a systematic review and meta-analysis PubMed Central
- Phillips SM et al, 2007, A critical examination of dietary protein requirements, benefits, and excesses in athletes PubMed
- Krieger JW, 2006, Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: a meta-regression The American Journal of Clinical Nutrition
- Fellström B et al, 1983, The influence of a high dietary intake of purine-rich animal protein on urinary urate excretion and supersaturation in renal stone disease PubMed
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) (2005)/11 Macronutrients and Healthful Diets The National Academic Press
- Choy HK et al, 2004, Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men The New England Journal of Medicine
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) (2005)/11 Macronutrients and Healthful Diets The National Academic Press
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) (2005)/11 Macronutrients and Healthful Diets The National Academic Press
- Friedman AN et al, 2012, Comparative Effects of Low-Carbohydrate High-Protein Versus Low-Fat Diets on the Kidney Clinical Journal of the American Society of Nephrology
- Hiatt RA et al, 1996, Randomized Controlled Trial of a Low Animal Protein, High Fiber Diet in the Prevention of Recurrent Calcium Oxalate Kidney Stones American Journal of Epidemiology
- Halton TL et al, 2004, The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review USDA Nutrition Evidence Library
- Dong JY et al, 2013, Effects of high-protein diets on body weight, glycaemic control, blood lipids and blood pressure in type 2 diabetes: meta-analysis of randomised controlled trials British Journal of Nutrition
- Lukas Schwingshackl L et al, 2013, Long-term effects of low-fat diets either low or high in protein on cardiovascular and metabolic risk factors: a systematic review and meta-analysis Nutrition Journal
- Altorf W et al, 2010, Dietary Protein and Blood Pressure: A Systematic Review Plos One
- Johnston CS et al, 2002, Postprandial thermogenesis is increased 100% on a high-protein, low-fat diet versus a high-carbohydrate, low-fat diet in healthy, young women PubMed
- Ascheson KJ et al, 2011, Protein choices targeting thermogenesis and metabolism The American Journal of Clinical Nutrition
- Westerterp KR, 2004, Diet induced thermogenesis Nutrition&Metabolism
- Bray GA et al, 2012, Effect of Dietary Protein Content on Weight Gain, Energy Expenditure, and Body Composition During Overeating: A Randomized Controlled Trial The Journal of the American Medical Association
- Pasiakos SM et al, 2013, Effects of high-protein diets on fat-free mass and muscle protein synthesis following weight loss: a randomized controlled trial The Journal of Federation of American Societies for Experimental Biology
- Appel LJ, 2003, The effects of protein intake on blood pressure and cardiovascular disease PubMed
- He J et al, 2011, Effect of Dietary Protein Supplementation on Blood Pressure Circulation
- Beekman T et al, 2013, The role of dietary protein in blood pressure regulation PubMed
- Buendia JR et al, 2014, Diets Higher in Protein Predict Lower High Blood Pressure Risk in Framingham Offspring Study Adults PubMed
- Robertson LM et al, 2009, Protein restriction for diabetic renal disease Cochrane Summaries
- Lönnerdal B, 2000, Dietary Factors Influencing Zinc Absorption The Journal of Nutrition
- Sandström B et al, 1989, Effect of Protein Level and Protein Source on Zinc Absorption in Humans The Journal of Nutrition
- Larsen RN et al, 2011, The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial PubMed
- Nezu U et al, 2013, Effect of low-protein diet on kidney function in diabetic nephropathy: meta-analysis of randomised controlled trials BMJ Open
- Nowlin SY et al, 2012, Diet, Inflammation, and Glycemic Control in Type 2 Diabetes: An Integrative Review of the Literature PubMed Central
- Fink HA et al, 2010, Diet, Fluid, or Supplements for Secondary Prevention of Nephrolithiasis: A Systematic Review and Meta-Analysis of Randomized Trials PubMed Central
- Nilsson LM et al, 2013, Low-carbohydrate, high-protein diet score and risk of incident cancer; a prospective cohort study Nutrition Journal
- What is the relationship between the intake of animal protein products and breast cancer? USDA Nutrition Evidence Library
- What is the relationship between the intake of animal protein products and colorectal cancer? USDA Nutrition Evidence Library
- What is the relationship between the intake of animal protein products and prostate cancer? USDA Nutrition Evidence Library
- Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate ( 2005 )/4 Water The National Academic Press
- Bilsborough S et al, 2006, A review of issues of dietary protein intake in humans PubMed
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) (2005)/10 Protein and Amino Acids The National Academic Press
- Franz MJ et al, 2002, Evidence-Based Nutrition Principles and Recommendations for the Treatment and Prevention of Diabetes and Related Complications Diabetes Care
- Deutz NEP et al, 2013, Is there a maximal anabolic response to protein intake with a meal? PubMed Central
- Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids US Department of Agriculture
- Estimated calorie requirements WebMD
- Ismail B et al, 2009, Whey Protein Hydrolysates: Current knowledge and Challenges Midwest Dairy Foods Research Center
- Pedersen AN et al, 2013, Health effects of protein intake in healthy adults: a systematic literature review PubMed Central
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA), 2010, Scientific Opinion on the substantiation of health claims related to whey protein and increase in satiety leading to a reduction in energy intake, contribution to the maintenance or achievement of a normal body weight, growth or maintenance of muscle mass, increase in lean body mass during energy restriction and resistance training, reduction of body fat mass during energy restriction and resistance training, increase in muscle strength, increase in endurance capacity during the subsequent exercise bout after strenuous exercise, skeletal muscle tissue repair and faster recovery from muscle fatigue after exercise European Food Safety Authority
- Sindayikengera S et al, 2006, Nutritional evaluation of caseins and whey proteins and their hydrolysates from Protamex PubMed Central
- Micke P et al, 2002, Effects of long-term supplementation with whey proteins on plasma glutathione levels of HIV-infected patients PubMed
- Whitt KN et al, 2008, Cholestatic liver injury associated with whey protein and creatine supplements PubMed
- Whey protein safety Mayo Clinic
- Lactose intolerance symptoms NHS Choices
- Milk composition; proteins University of Illinois
- Osborn DA et al, 2009, Formulas containing hydrolysed protein for prevention of allergy and food intolerance in infants Cochrane Summaries
- Camilleri G et al, 2013, Plant and Animal Protein Intakes Are Differently Associated with Nutrient Adequacy of the Diet of French Adults The Journal of Nutrition
- van der Kuil WA et al, 2010, Dietary Protein and Blood Pressure: A Systematic Review PubMed Central
- What is the relationship between the intake of soy protein and blood lipids among adults without hyperlipidemia? (DGAC 2010) USDA Nutrition Evidence Library
- What is the relationship between the intake of animal protein products and colorectal cancer? (DGAC 2010) USDA Nutrition Evidence Library
- Foods highest in protein Nutritiondata
- Young VR et al, 1994, Plant proteins in relation to human protein and amino acid nutrition The American Journal of Clinical Nutrition
- Digestive System State University of New York, Clinton Community College
- Dangin M et al, 2002, Influence of the Protein Digestion Rate on Protein Turnover in Young and Elderly Subjects The Journal of Nutrition
- Absorption of amino acids and peptides Colorado State University
- Manninen AH, 2004, Protein Hydrolysates in Sports and Exercise: A Brief Review PubMed Central
- Overview of malabsorption Merck Manuals
- Pancreatic enzyme replacement Pancreaticcanceraction.org
- Protein-losing enteropathy clinical presentation Emedicine
- Pasiakos SM et al, 2014, Effects of protein supplements on muscle damage, soreness and recovery of muscle function and physical performance: a systematic review PubMed
- Cermak NM et al, 2012, Protein supplementation augments the adaptive response of skeletal muscle to resistance-type exercise training: a meta-analysis The American Journal of Clinical Nutrition
- Calbet JAL et al, 2002, Plasma Glucagon and Insulin Responses Depend on the Rate of Appearance of Amino Acids after Ingestion of Different Protein Solutions in Humans The Journal of Nutrition
- Overview of protein metabolism Elmhurst College
- Evenepoel P et al, 1999, Amount and fate of egg protein escaping assimilation in the small intestine of humans Gastrointestinal and Liver Physiology
- Evenepoel P et al, 1998, Digestibility of Cooked and Raw Egg Protein in Humans as Assessed by Stable Isotope Techniques The Journal of Nutrition
- Sweetman L et al, 1981, Clinical and metabolic abnormalities in a boy with dietary deficiency of biotin PubMed
- Biotin deficiency Emedicine
- Gill P et al, 2011, Beef: Correlation between Physical Properties and Quality Worchester Polytechnic Institute
- Robertson WG, 2003, Renal stones in the tropics PubMed
- Diet for kidney stone prevention National Institute of Diabetes and Digestive and Kidney Diseases
- Cereda E et al, 2010, Low-protein and protein-redistribution diets for Parkinson’s disease patients with motor fluctuations: a systematic review PubMed
- Fouque D et al, 2009, Low protein diets for chronic kidney disease in non diabetic adults PubMed
- Kidney Failure: Eat Right to Feel Right on Hemodialysis National Institute of Diabetes and Digestive and Kidney Diseases
- Fouque D et al, 2000, Low protein diets delay end-stage renal disease in non diabetic adults with chronic renal failure PubMed
- Vendrely B et al, 2003, Nutrition in hemodialysis patients previously on a supplemented very low protein diet PubMed
- Chantal B et al, 2010, Role of Nutrition in the Management of Hepatic Encephalopathy in End-Stage Liver Failure PubMed Central
- Poh Z et al, 2012, A Current Review of the Diagnostic and Treatment Strategies of Hepatic Encephalopathy PubMed Central
- Wright G et al, 2011, Management of Hepatic Encephalopathy PubMed Central
- Siener R et al, 2003, The effect of a vegetarian and different omnivorous diets on urinary risk factors for uric acid stone formation PubMed
- Taylor EN et al, 2004, Dietary Factors and the Risk of Incident Kidney Stones in Men: New Insights after 14 Years of Follow-up Journal of the American Society of Nephrology
- Speth JD, 2010, The Paleoanthropology and Archaeology of Big-Game Hunting: Protein, Fat, or Politics?
- Rexford S. Ahima, 2011, Metabolic basis of obesity
- LTC Robert B Lim et al, 2011, Benchmarking Best Practices in Weight Loss Surgery PubMed Central
- Watson RR, Handbook of Nutrition in the Aged, Fourth Edition
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) ( 2005 ) / 10 Protein and Amino Acids US Department of Agriculture
- Protein-Energy Malnutrition Clinical Presentation Emedicine
- Protein-Energy Malnutrition Treatment and Management Emedicine
- Fryburg DA et al, 1995, Insulin and Insulin-like Growth Factor-I Enhance Human Skeletal Muscle Protein Anabolism during Hyperaminoacidemia by Different Mechanisms PubMed Central
- Franz MJ, 1997, Protein: metabolism and effect on blood glucose levels PubMed
- Fouque D et al, 2009, Low protein diets can delay kidney failure in people with kidney disease (diabetic kidney disease excluded) Cochrane Summaries
- Rooyackers OE et al, 1997, Hormonal regulation of human muscle protein metabolism PubMed
- Pasiakos SM et al, The Effects of Protein Supplements on Muscle Mass, Strength, and Aerobic and Anaerobic Power in Healthy Adults: A Systematic Review PubMed
- Protein Intolerance Emedicine
- Untersmayr E et al, 2008, The role of protein digestibility and antacids on food allergy outcomes PubMed Central
- Guidelines for the Diagnosis and Management of Food Allergy in the United States National Institute of Allergy and Infectious Diseases
- Stearns RL et al, 2010, Effects of ingesting protein in combination with carbohydrate during exercise on endurance performance: a systematic review with meta-analysis PubMed
- McLellan TM et al, 2014, Effects of protein in combination with carbohydrate supplements on acute or repeat endurance exercise performance: a systematic review PubMed
- Amino Acid Injection Drugs.com
- Amino acid-based nutritional supplement Drugs.com
- Nutrient bioavailability – getting the most out of food European Food Information Council
- Caspero A, Protein and the Athlete – How Much Do You Need? Academy of Nutrition and Dietetics
- The 2015 Prohibited List, International Standard World Anti-Doping Agency
- Protein Australian Sports Commission
- Phillips SM et al, 2011, Dietary protein for athletes: from requirements to optimum adaptation PubMed
- Kerndt PR et al, 1982, Fasting: The History, Pathophysiology and Complications The Western Journal of Medicine
- Owen OE et al, 1998, Protein, fat, and carbohydrate requirements during starvation: anaplerosis and cataplerosis The American Journal of Clinical Nutrition
- Lieberson AD, 2004, How long can a person survive without food? Scientific American
- Mangels R, Protein in the Vegan Diet The Vegetarian Resource Group
- Hypoalbuminemia, Clinical Presentation Emedicine
- Hypoalbuminemia, Workup Emedicine
- Differential Diagnosis For Hypoalbuminemia Hypoproteinemia – Causes, Anemia in Elderly – Causes, Macrocytic anemia (Lab) DiagnosisPro
- Albumin, Human Drugs.com
- Schwartz R et al, 1973, Metabolic responses of adolescent boys to two levels of dietary magnesium and protein. I. Magnesium and nitrogen retention The American Journal of Clinical Nutrition
- Protein Synthesis Sparknotes
- Villareal DT et al, 2012, Effect of weight loss on the rate of muscle protein synthesis during fasted and fed conditions in obese older adults PubMed Central
- Layman DK et al, 2005, Dietary Protein and Exercise Have Additive Effects on Body Composition during Weight Loss in Adult Women The Journal of Nutrition
- Vishwanath Sardesai, 2012, Introduction to Clinical Nutrition, Third Edition
- Poth EJ et al, 1965, Digestion and Absorption following Gastrectomy Using Reversed Jejunal Segments: Follow Up of 50 Cases PubMed Central
- Manninen AH, 2006, Very-low-carbohydrate diets and preservation of muscle mass PubMed Central
- Young LR et al, 2013, Low-fat diet with omega-3 fatty acids increases plasma insulin-like growth factor concentration in healthy postmenopausal women National Agricultural Library
- Rietman A et al, 2014, High dietary protein intake, reducing or eliciting insulin resistance? PubMed
- Zhu K et al, 2011, The effects of a two-year randomized, controlled trial of whey protein supplementation on bone structure, IGF-1, and urinary calcium excretion in older postmenopausal women PubMed
- What is the relationship between the intake of animal protein products and type 2 diabetes? (DGAC 2010) USDA Nutrition Evidence Library
- Morenga LAT et al, 2011, Comparison of high protein and high fiber weight-loss diets in women with risk factors for the metabolic syndrome: a randomized trial Annual Reviews
- Hoffman JR et al, 2009, Effect of protein-supplement timing on strength, power, and body-composition changes in resistance-trained men PubMed
- Helms ER et al, 2014, A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: a case for higher intakes PubMed
- Esmarck B et al, 2001, Timing of postexercise protein intake is important for muscle hypertrophy with resistance training in elderly humans Journal of Physiology
- Biolo G et al, 1997, An abundant supply of amino acids enhances the metabolic effect of exercise on muscle protein PubMed
Proteins
What are proteins?
Proteins are macronutrients made of amino acids. They are essential nutrients found in both animal and plant foods.
The name protein originates from the Greek proteios, which means “first quality” [1].
Nutrition Facts
- Calories per gram = 4 Cal of “metabolizable energy” or 3.2 Cal of “net metabolizable energy”
- Cooked proteins (meat, eggs) are digested easier than raw proteins.
Functions of Proteins and Their Importance in the Human Body
1. Dietary Protein as a Source of Energy
The calorie value for protein on the Nutrition Facts labels of foods is 4 Calories per gram, which represents “metabolizable energy,” which can be used by the human body. But if we distract the energy used to digest, absorb and metabolize protein, we get 3.2 Calories per gram of “net metabolizable energy,” which can be converted to physical energy or body weight [2,3]. Net metabolizable energies for carbohydrates (4 Cal/g) and fats (9 Cal/g) are practically the same as their metabolizable energies [2,3].
2. Proteins in the Human Body
Dietary proteins provide building blocks–amino acids–for proteins in the human body:
- Structural proteins: Collagen gives the structure to the bones, skin and connective tissue (tendons and ligaments); elastin gives elasticity to the skin; keratin gives structures to the nails and hair; keratin is also in the upper layer of the skin; actin and myosin enable muscle contraction, and cell membrane proteins regulate influx and outflux of certain substances into and out from the cells.
- Transport proteins: Hemoglobin carries oxygen, and transferrin carries iron in the blood; myoglobin carries oxygen in the muscles; ferritin stores iron, and cytochromes carry electrons in the respiratory chain in the cells; albumin carries certain ions, hormones, vitamins, bilirubin, drugs and toxins via the blood. Albumin also helps to retain water in the blood.
- Enzymes enable synthesis or breakdown of most substances in the body.
- Thrombin and fibrin enable blood coagulation; fibrin also enables wound healing.
- The hormones insulin, oxytocin, somatotropin and thyroxine are proteins.
- Proteins released into the blood in inflammation: C-reactive protein, prostaglandins, prostacyclins.
- Antibodies (immunoglobulins IgA, IgE, IgG, IgM) enable defense against microbes (immunity).
Protein deficiency can affect all above functions.
Synthesis of proteins in the human body is regulated by DNA [129].
How many grams of protein do you need per day?
According to the Institute of Medicine (IMO) in the U.S., the Recommended Dietary Allowance (RDA) for protein is 0.8 g/kg or 0.36 g/lb body weight per day; in average 56 g/day for men and 46 g/day for women [4]. The Acceptable Macronutrient Distribution Range (AMDR) for protein for adults is 10-35% of total calories consumed or 50-175 g/day [4].
Chart 1. RDA and AMDR for Protein |
||
Age |
RDAGrams/day for average body weight |
AMDRGrams/day |
| 0–6 months | 9 g/day (1.5 g/kg) [Adequate Intake] | Not determinable |
| 7–12 months | 11 g/day (1.5 g/kg) | Not determinable |
| 1–3 years | 13 g/day (1.1 g/kg) | 10-50 g/day (5-20% of 1,000 Cal) |
| 4–8 years | 19 g/day (0.95 g/kg) | 30-100 g/day (10-30% of 1,300 Cal)** |
| 9–13 years | 34 g/day (0.95 g/kg) | 40-130 g/day (10-30% of 1,700 Cal)** |
| Boys 14-18 years | 52 g/day (0.8 g/kg) | 55-175 g/day (10-30% of 2,200 Cal)** |
| Girls 14-18 years | 46 g/day (0.8 g/kg) | 45-135 g/day (10-30% of 1,800 Cal) |
| Men 19-50 | 56 g/day (0.8 g/kg) | 55-190 g/day (10-35% of 2,200 Cal) |
| Women 19-50 | 46 g/day (0.8 g/kg) | 45-160 g/day (10-35% of 1,800 Cal) |
| Pregnant and breastfeeding women | 71 g/day (1.1 g/kg) | 60-210 g/day (10-35% of 2,400 Cal) |
Chart 1 source: Adapted from Institute Of Medicine [4], US Department of Agriculture [50-pp.176-178] and WebMD [51] ** The lower AMDR values in age groups 4-18 years seem to be set too high.
Minimal Required Amount of Protein
According to one estimation, adults need to consume at least about 35 grams of protein per day [97-p.324] in order to get enough essential amino acids and nitrogen for the synthesis of the body proteins, DNA and RNA (parts of chromosomes).
How long can you live without protein?
According to various reports, people have survived for more than 40 days without food and hence without protein [121]. After prolonged starvation, people can die even before their fat stores are depleted, probably due to deficiency of essential amino acids [121]. Losing 1/3 to 1/2 of the body protein, which is about 3 kg of muscle mass, may be incompatible with life [120].
Protein Requirements for Athletes
According to Food and Nutrition Research journal, there is INCONCLUSIVE EVIDENCE about protein requirements during physical training [53], but various researchers have made estimations about appropriate daily intakes of protein for athletes:
- For recreational endurance athletes: 0.8-1 g/kg body weight [118]
- For professional endurance athletes: 1.2-1.4 g/kg body weight [12,116]
- For resistance training, when gaining muscle: 1.6-1.7 [12] and to maintain the muscle mass: 1-1.2 g/kg body weight [118]
- To maintain muscle mass in athletes during calorie-deficit diet: 1.8-2 g/kg body weight [119] or even 2.3-3.1 g/kg of fat free mass [141].
Protein Timing
There is INCONCLUSIVE EVIDENCE about the importance of the time of protein ingestion on muscle mass gain and strength in resistance-trained athletes: from no effect of the ingestion time [140] to greater effect if ingested immediately after exercise than when ingested at some later time [142,143].
While some researchers believe, the maximum amount of protein in one meal that can stimulate protein synthesis is 20-30 grams, others believe no such maximum exists [49].
Calorie-Restricted Diet and Muscle Mass Loss
During calorie-restricted diet for weight loss, the synthesis of the muscle protein is not impaired but its breakdown is increased, which can result in a decrease of muscle mass [130].
A combination of a high-protein low-carbohydrate diet and exercise during weight loss can help prevent muscle mass loss [131,134].
High blood levels of amino acids (hyperaminoacidemia) and hormones insulin inhibit muscle protein breakdown; growth hormone, insulin-like growth factor (IGF-I or somatomedin C) and testosterone stimulate protein synthesis [103,106]. Glucagon and thyroxine stimulate muscle protein breakdown [106].
Protein Sources
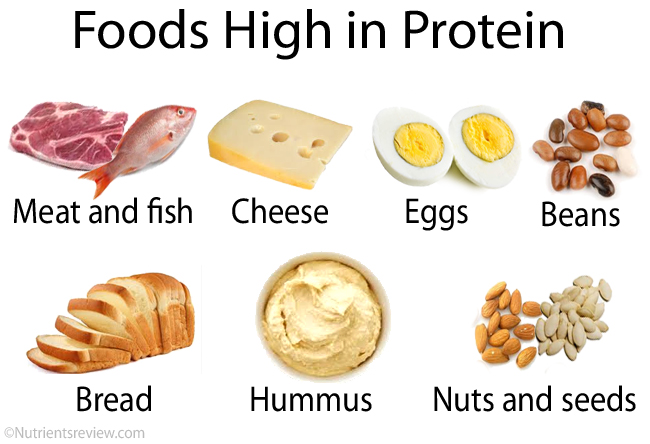
Picture 1. Examples of foods high in protein
Chart 2. Foods High in Protein |
||
ANIMAL FOODS |
Protein (g) |
Comments |
| Meat/fish (3 oz, 85 g): bacon (cured), salmon (red, sockeye) | 29-30 | |
| Lean meats, cooked (3 oz, 85 g): beef, buffalo, caribou, chicken, deer, duck, elk, emu, goat, goose, ham, lamb, ostrich, pork, rabbit, turkey | 20-27 | Certain beef, pork, duck and goose cuts are lean |
| Fish, cooked (3 oz, 85 g): grouper, haddock, herring (Atlantic), mackerel, octopus, salmon, sardines, sea bass, tilapia, tilefish, tuna | 20-25 | Big fish from the Gulf of Mexico (king mackerel, shark, swordfish, tilefish, tuna) may be high in mercury or other toxins. |
| Organ meats (3, oz, 85): liver, kidney, spleen | ~20 | High in cholesterol |
| Seafood, cooked (3 oz, 85 g): carp, cod, crab, crayfish, halibut, lobster, pollock (Alaska), shark, shrimps, trout, tuna (light) | 15-20 | Shrimps are high in cholesterol |
| Cheese (2 oz, 57 g): goat, gruyere, romano, Swiss | 16-18 | |
| Dairy (1 cup, 237 mL): sheep milk, Greek yogurt | 15 | |
| Cheese (2 oz, 57 g): american pasteurized, blue, brick, brie, camembert caraway, cheddar, cheshire, colby, edam, fontina, gouda, limburger, monterey, mozzarella, muenster, pimento pasteurized, port de salut, provolone, queso anejo, rocquefort, tilsit | 12-14 | |
| Milk (1 cup, 237 mL): cow, buffalo milk | 8-9 | High in lactose |
| Cheese (2 oz, 57 g): cottage, creamed, feta, fondue, gjetost, neufchatel, ricotta | 6-8 | |
| Egg, whole (50 g) | 6 | High in cholesterol |
| Egg, white only (33 g) | 4 | |
| Whey, dried (1 oz, 4 tbsp or 1 scoop 28 g) | 4 | Can be high in lactose |
PLANT FOODS |
||
| Soy protein isolate (1 oz, 28 g) | 25 | Can have bitter taste |
| Seitan, wheat gluten (1 oz, 28 g) | 21 | |
| Protein bar, example (2.8 oz, 80 g) | 20 | |
| Soybeans, cooked (1/2 cup, 120 mL) | 11 | |
| Cereals, cooked (1 cup, 237 mL): amaranth, cornmeal, kamut, pasta, quinoa; bagel (3″), bread (2 slices, 60 g) | 8-11 | |
| Hummus dip (1/2 cup, 120 mL) | 10 | |
| Tempeh (2 oz, 57 g) | 10 | |
| Tofu, firm (1/2 cup, 120 mL) | 10 | |
| Hemp seeds, hulled (1 oz, 28 g) | 10 | |
| Legumes, cooked (1/2 cup, 120 mL): beans, edamame, lentils, peas (chickpeas, split peas) | 6-9 | Can cause bloating |
| Seeds, kernels (1 oz, 28 g): cottonseed, pumpkin, safflower, sesame, squash, sunflower | 5-9 | |
| Peanut butter (2 tbsp, 32 g) | 8 | |
| Vegetables, cooked: taro (1 cup) | 5-8 | |
| Protein bread (2 slices, 60 g) | 7 | |
| Cereals, cooked (1 cup, 237 mL): bulgur, buckwheat, millet, oatmeal; rye bread (2 slices, 60 g) | 6 | |
| Nuts (1 oz, 28 g): almonds, cashews, peanuts, pistachios, walnuts (black) | 6 | |
| Miso (2 oz, 57 g) | 6 | |
| Tahini ─ sesame seed spread (1 oz, 28 g) | 5 | |
| Soy milk (1 cup, 237 mL) | 5 | |
| Rice, white or brown, cooked (1 cup, 237 mL) | 5 | |
OTHER FOODS |
||
| Mycoprotein (100 g) [7] | 11 | |
| Yeast extract (2 tbsp, 32 g) | 8 | |
Chart 2 source: USDA.gov [6]
Foods containing 2-5 grams of protein per serving [6]:
- Vegetables, cooked (1/2 cup, 120 mL): broccoli, Brussel’s sprouts, cabbage, cauliflower, corn (sweet), mushrooms, onion, pepper (green), spinach, tomato, turnip greens; potato and sweet potato (1 cup), yam (1 cup)
- Green peas (1/2 cup, 120 mL)
- Avocado (1 cup)
- Seeds, nuts (1 oz, 28 g): brazilnuts, cashews, chia seeds, hazelnuts, macadamia nuts, pecans, pine nuts; chestnuts (100 g)
- Cereals, cooked (1 cup, 237 mL): barley
- Other: ice cream (1/2 cup, 120 mL), pudding (1 cup, 237 mL), oatmeal cookies or wheat crackers (2 oz, 57 g), chocolate (1 oz)
Plant vs Animal Protein
In various studies, in general, plant protein was associated with less health risk than animal protein [53,62], but the direct cause-effect relationship between plant protein and health risks has not been proven.
According to some systematic reviews of studies, there is INSUFFICIENT EVIDENCE that animal protein would be more beneficial or harmful for human health than plant protein:
- There is insufficient evidence about the effect of soy protein intake on total and LDL cholesterol levels [53,64].
- There is a small and inconsistent evidence about the association between the intake of red and processed meat and colorectal cancer [65].
- There is inconclusive evidence about the association between the intake of animal protein and kidney stones [95].
- High intake of total protein or animal protein was not associated with gout [16].
- Limited inconsistent evidence from prospective cohort studies suggests that intake of animal protein products, mainly processed meat, may be associated with diabetes mellitus type 2 [138].
Complete or “Good” or “High Quality” vs Incomplete Protein
Foods with complete protein contain all 9 essential amino acids in sufficient amounts to meet the body needs. Most animal foods and some plant foods: amaranth, avocado, buckwheat, chestnuts, certain legumes (certain beans, chickpeas or Garbanzo beans, split peas, soy), pistachios, potatoes, pumpkin seeds, quinoa, a seaweed spirulina, spinach, tofu and hummus contain complete protein [66].
Some plant foods contain incomplete protein, which means they are low in certain essential amino acids [66]. Plant foods with incomplete protein do not need to be called “low quality” protein sources because their combining can provide sufficient amount of all essential amino acids to meet the body needs.
Complementary Proteins and Protein Combining
Complementary protein foods are foods that are low in certain essential amino acids, but in combination, provide all 9 essential amino acids in amounts that allow synthesis of adequate amounts of protein in the human body. Examples of complementary protein foods are cereal grains, nuts and seeds, which tend to be low in lysine and tryptophan, but high in methionine, in combination with legumes, which tend to be high in lysine and tryptophan but low in methionine. Complementary proteins do not need to be eaten in the same meal or even not in the same day, but, according to The American Journal of Clinical Nutrition, “over number of days” [67]. They are usually only vegans who need to think about complementing proteins.
Can vegans get enough protein?
Vegans, who do not eat meat, fish, eggs and milk products, can get enough protein by eating nuts, seeds, legumes, bread, rice and other plant foods high in protein (Chart 2). Various protein bars, meatless products (meat substitutes), seitan (wheat gluten), vegan protein shakes and other protein products are available. Healthy vegans who eat variety of plant foods in sufficient amounts do not likely need protein supplements [123].
Protein Digestion and Absorption
Digestion
In order to be absorbed, proteins have to be digested (broken down) to amino acids.
The enzyme pepsin in the stomach and the enzymes trypsin and chymotrypsin, produced by the pancreas and delivered to the small intestine by pancreatic juice, break down protein to short chains of amino acids. The enzymes peptidases in the small intestinal lining further break down chains of amino acids to either single amino acids or compounds of 2 (dipeptides) or 3 amino acids (tripeptides), which can all be absorbed [68,70]. Exceptionally, mainly in newborns, some intact food proteins can be absorbed [70].
The Absorption Rate
The estimated absorption rate for protein (amino acids) is 1.3-10 grams per hour [46], depending on the type of protein. Whey protein (from milk) is digested and absorbed faster than casein (from milk) and most other dietary proteins [69]. Protein hydrolysates (supplements with short chains of amino acids) are absorbed faster than free amino acids or whole proteins [71,77]. The eventual upper limit for protein absorption is not known; according to European Food Information Council, more than 90% of the ingested protein should be absorbed [115].
Protein Maldigestion and Malabsorption
Protein digestion and absorption can be impaired in certain pancreatic and intestinal disorders, such as pancreatitis, pancreatic cancer, partial surgical removal of the pancreas or small intestine, celiac or Crohn’s disease, intestinal lymphoma or tuberculosis and cystic fibrosis [72]. Low gastric acid secretion (achlorhydria or hypochlorhydria) probably do not significantly affect protein digestion [132-p.33; 133].
Severe protein malabsorption can lead to low blood protein levels (hypoproteinemia or hypoalbuminemia) and body swelling (edema) [72].
Supplemental pancreatic enzymes, usually as capsules that contain enzymes required to digest proteins (trypsin), fats (lipase) and carbohydrates (amylase), are available by prescription or over the counter.
Protein Metabolism
The fate of dietary protein after absorption
When amino acids (breakdown products of protein digestion) are absorbed into the blood, they enter liver, muscle and other body cells, where they can be converted to muscle and other body proteins, glucose or further to glycogen (a storage form of glucose in the liver and muscles), fatty acids or further to ketones (a source of energy for the brain during low-carb diet) or body fat stores, or can be converted to energy (physical, chemical and thermal) [78]. The excessive protein nitrogen is excreted in the form of urea in urine.
What will happen with protein you consume depends on circumstances:
- When you consume more calories than you spend, some protein will be converted to the body fat.
- In a low-carbohydrate, high-protein diet, some protein will be used for energy for your body, some will be converted to glucose and some to ketones, both of which can be used as a source of energy for the brain.
- During resistance training, some protein will be converted to muscle proteins, which will increase your muscle mass. Some researchers believe that Recommended Dietary Allowance for protein (0.8 g/kg body weight for adults) is enough to build muscles during resistance training.
Cooked vs Raw Protein
During cooking, protein undergoes denaturation ─ a physical change that makes it easier to digest. During denaturation, protein does not break down to amino acids and its calorie value does not change significantly.
Cooked vs Raw Eggs
- 30-40% less protein may be absorbed from raw than from cooked eggs [79,80].
- Regular consumption of raw egg whites, which contain a protein avidin, which can bind the vitamin biotin, can result in biotin deficiency; avidin from cooked egg whites does not bind biotin [81,82].
Raw vs Cooked Meat
- Cooked meat is digested easier than raw meat.
- Meat protein denaturates at about 84° C (183° F) [83].
Raw vs Cooked Milk
Raw and cooked milk protein are probably digested at about the same rate.
High-Protein Diet
Possible Benefits
CONVINCING EVIDENCE:
- The body’s heat production (thermogenesis). The thermic effect of a high-protein meal can be as much as twice higher than of a high-carbohydrate meal [21,25,26,27].
SOME EVIDENCE:
- Lower body fat percent. In various studies, high-protein, calorie-deficient diets were associated with greater percentage of body fat loss than low-protein diets [13,21,29]. Inconclusive for body composition [53].
- Decrease of high blood pressure. There is some evidence that a high-protein diet and diet high in plant protein are associated with a slight decrease of blood pressure [11,30,31,32,33,63].
There is INSUFFICIENT EVIDENCE about the effect of high-protein diet on
- Weight loss. There is some evidence that high-protein diet can increase satiety but insufficient evidence about its long-term (>1 year) effect on weight loss [10,11,18,19,21,27,53].
- For patients with end-stage liver disease with hepatic encephalopathy, some authors recommend 1.2-1.5 g protein/day, preferably vegetable protein, except to those with severe protein intolerance [91,92,93].
Is too much protein bad for you? Possible Side Effects and Dangers
SOME EVIDENCE:
- Gastrointestinal problems. According to some, but not all studies, in some individuals, high-protein diets can be associated with bad breath (halitosis), diarrhea, bloating and, when a diet is low in fiber, constipation [11].
INSUFFICIENT EVIDENCE:
- Impaired kidney function. In healthy people, high-protein diet or protein supplements, like whey, probably do not impair kidney function or cause kidney damage [9,17,19,21,53].
- Kidney stones. In healthy people, high-protein diet alone does not likely increase the risk of kidney stones [9,19,20,40,53]. In high protein diet, urine is more acidic, higher in calcium and urate but this is probably not enough to form calcium or urate kidney stones [9,14]. In individuals with certain metabolic disorders, high-protein diet, especially diet high in animal protein (meat, organ meats, fish, eggs), can increase the risk of urate and cystine kidney stones, though [9,85].
- Diabetes mellitus type 2. In some, but not all, studies, high-protein diet was associated with increased risk of diabetes 2 [136,139].
- Osteoporosis. A high-protein diet results in increased calcium excretion in urine, but it does not likely increases the risk of osteoporosis (low bone density) [15,19,53].
- Heart disease. High protein intake does not likely increase the risk of coronary artery disease and high blood pressure [9,11,17,23,24,53].
- Inflammation. Neither high- nor low-protein diet are consistently associated with inflammation (concluded from insignificant changes in blood C-Reactive Protein or CRP levels) [11,39].
- Cancer. There is insufficient evidence about association between diets high in protein or animal protein and the risk of breast, prostate, colorectal or other cancer [18,41,42,43,44,53].
- The long-term (>20 years) effects of a high-protein, low-carbohydrate diets on health are not known [48].
Effect of High-Protein Diet on Blood Lipids
In various studies, high-protein diet was associated with slightly lower blood triglyceride, lower LDL and slightly higher HDL cholesterol levels [11,17,22,23,37].
How much protein is too much?
To date, the exact maximum safe protein intake for healthy individuals is not known.
- The Institute Of Medicine in the U.S. has not established the Tolerable Upper Intake Level (UI) for protein [50].
- According to one study, the human kidneys of adults can excrete only the amount of protein metabolic products (urea) that corresponds to ingestion of about 250 g protein/day by a 70 kg person, but this maximum may increase during a long-term high-protein diet [50-p.694].
- According to one source, a suggested maximum protein intake for an 80 kg person on a 2,800 Calorie diet is 2-2.5 g/kg body weight per day or 176 g/day [46] and “theoretical maximum safe intake” for an 80 kg person is 285-365 g/day [46].
“Protein Poisoning” or “Rabbit Starvation Syndrome” or “Mal de Caribou”
The human liver has a limited capacity to metabolize proteins, so excessive protein intake (> 35% of total calorie intake) may result in increased blood levels of amino acids (hyperaminoacidemia), ammonium (hyperammonemia) and insulin (hyperinsulinemia), and even death [46].
According to an explorer Stefansson (in 1940s and 1950s), several weeks of eating only lean meat, such as rabbit or caribou meat, which contains very little fat, and eating no other food, can result in death due to so called “rabbit starvation syndrome” [47,96]. One adult man consuming about 45% calories from protein for more than a week has experienced weakness, hunger, nausea and diarrhea, which were resolved by increasing fat intake and reducing protein intake to 20-25% calories [47]. On the other hand, according to several reports, eating only meat or pemmican (dried meat with added fat) containing 20-35% calories from protein and the rest from fat for “extended periods” did not cause any adverse effects [47].
Food Protein Intolerance (Allergy)
Food protein intolerance is an adverse reaction to protein with one or more gastrointestinal symptoms (burning mouth, nausea, vomiting, abdominal pain, constipation or diarrhea), skin rash (hives, eczema), runny nose, difficulty breathing or wheezing occurring within few minutes to hours after food ingestion. Food protein allergy is a type of protein intolerance with increased release of IgE antibodies.
Cow’s milk, soybean and eggs are most common triggers of protein intolerance in children; intolerances often resolve before age of five but may, rarely, persist into adulthood. Practically any other food, including meats, fish, shellfish, nuts, seeds and foods that contain very little protein, such as fruits, vegetables and oils, can be involved in protein intolerance. Intolerances to more than one protein are possible; infants with cow’s milk intolerance are often intolerant to soy protein.
Disorders related to protein intolerance include oral allergy syndrome, immediate gastrointestinal hypersensitivity, eosinophilic esophagitis, gastritis and gastroenteritis; enterocolitis, protein-losing enteropathy, proctocolitis, chronic constipation (as the sole symptom), atopic dermatitis, multiple food protein intolerance of infancy (to several foods, including breast milk) and celiac disease (adverse reaction to gluten). In infants with cow’s milk intolerance, rarely, anaphylactic shock (pale, sweaty, cold skin) due to a sudden drop of blood pressure can develop.
Decreased secretion of gastric acid (hypochlorhydria) or using gastric acid lowering drugs (antacids, H2 blockers, proton pump inhibitors) increases the risk of protein allergies, because a lower amount of acid in the stomach allows more intact proteins to pass into the intestine [109].
Diagnostic tests can include skin tests with food extracts, food eliminating and oral challenging tests, blood IgE levels, leukocytes in the stool, endoscopy with biopsy of the GI tract lining, etc.
Treatment possibilities: elimination of the offending food, exclusive breastfeeding instead of bottle feeding, free amino acids-based formula, antihistamines, corticosteroids; in case of anaphylactic shock: epinephrine injection into a muscle. Cooking fruits, vegetables and oils, but less likely other foods, can make them less allergenic [110].
References: [108]
Low-Protein Diet
If you have a kidney, metabolic or other disease, your doctor may prescribe you a low-protein diet.
Chart 3. A Low-Protein Diet |
|
| FOODS TO LIMIT | USUALLY NO NEED TO RESTRICT |
>20 g protein/serving:
|
5-10 g protein/serving
2-5 g protein/serving:
|
10-20 g protein/serving:
|
|
Chart 3 sources: USDA.gov [6]. NOTE: The above chart is for general information only; it is your doctor or dietitian who can tell how much protein you personally can eat.
A low-protein diet (0.6-0.8 g or less per kg body weight) is EFFECTIVE in:
- Individuals with certain genetic metabolic diseases, certain amino acids accumulate in the blood, so they should have a diet low in those amino acids.
A low-protein diet (0.6-0.8 g or less per kg body weight) is PROBABLY EFFECTIVE in the following disorders:
- In kidney failure, in which a breakdown of protein metabolism (urea) accumulates in the blood (uremia), a low-protein diet was associated with a decreased risk of death due to kidney disease [87,89,105]. However, patients on hemodialysis are usually advised to consume more protein, which can help them maintain muscle mass and stimulate tissue repair [88,90].
- Low-protein diet or diet low in animal protein can help prevent recurrence of urate kidney stones [85,94].
There is INSUFFICIENT EVIDENCE about the effectiveness of low-protein diets on:
- Improvement of symptoms of Parkinson’s disease [86].
Low-Protein Diet Safety: Dangers, Side Effects
A diet low in animal protein and high in cereals can increase the risk of ammonium acid urate bladder stones in children, mainly in tropical areas with poor nutrition [84].
Low-protein diet can result in loss of muscle mass
Protein and Diabetes
Results of studies in individuals with diabetes mellitus type 1 or 2:
- According to one 2002 review of studies, protein added to carbohydrate meals probably does not slow glucose absorption [48].
- Protein meals do not increase blood glucose levels after the meals [48,104].
- In various studies in individuals with diabetes mellitus 2, long-term (at least 1 year) high-protein diets did not result in a significantly different glycated hemoglobin (HbA1c) than high-carbohydrate diets [11,22,37].
- A low-protein diet may slightly slow down the progression of kidney disease in individuals with diabetes mellitus type 1 or 2 [34,38].
Protein Deficiency
In order to maintain nitrogen balance an adult has to consume at least about 35 grams of protein per day [97-p.324].
In the western world, the main causes of protein deficiency include:
- Low protein intake in anorexia nervosa, fad diets, food allergies, involuntary weight loss in care institutions, neuromuscular diseases, poor appetite in ill elderly people in nursing homes or, rarely, an unbalanced vegan diet
- Impaired protein digestion due to chronic pancreatic disorders
- Decreased protein absorption due to small intestinal disorders: severe gastrointestinal infections, intestinal parasites, celiac disease, Crohn’s disease, Whipple disease, lymphoma, intestinal tuberculosis, cystic fibrosis, surgical removal of a large part of the small intestine in infants (short bowel syndrome or SBS) or other disorders with severe diarrhea.
- Loss of protein through the gut–protein-losing enteropathy–as small intestinal bacterial overgrowth (SIBO), intestinal parasites, celiac disease, Crohn’s disease, ulcerative or pseudomembranous colitis, HIV/AIDS, tuberculosis, amyloidosis, systemic sclerosis and lymphoma [74].
- Increased protein loss in urine in individuals with untreated chronic kidney disease (nephrotic syndrome), or in those on hemodialysis
- Decreased protein synthesis in alcoholic liver cirrhosis
- Increased protein metabolism in cancer
- Weigh loss bypass surgery [98]
Protein-Energy Malnutrition (PEM): Kwashiorkor and Marasmus
Severe protein deficiency due to lack of protein in the diet may be still a problem in southern parts of African and Asia.
Kwashiorkor, which in the Ga language of Ghana means “the sickness of weaning,” is a protein deficiency without a calorie deficiency. It mainly affects small children after stopping breastfeeding, who get enough carbohydrates, but not enough proteins with food.
Marasmus, from Greek marasmos = wasting, is a combination of protein and calorie deficiency. The main cause is prolonged starvation.
Symptoms and Signs
- In children: slow growth, swollen abdomen (potbelly), dark, dry skin with pale cracks (“lacquer flaky paint”), hair with darker and brighter segments, skin ulcers, diarrhea
- In children and adults: fatigue, apathy, feeling cold due to decreased body temperature, low body weight, facial or feet swelling or abdominal distension (in liver cirrhosis), enlarged liver and spleen, loss of underskin fat, muscle wasting, hair loss, slow wound healing
- Protein deficiency in pregnant women may result in low birth weight and impaired brain development in infants.
Diagnosis of Protein Deficiency
- Blood tests: decreased levels of total protein (hypoproteinemia) or albumin (hypoalbuminemia; [99]), blood urea nitrogen (BUN), transferrin, glucose (hypoglycemia), cholesterol, iron, potassium, magnesium, calcium, phosphate, vitamins and decreased lymphocyte count.
- Urine tests: low urea levels, increased level of 3-metylhistidine – a breakdown product of muscle proteins (in marasmus)
- Stool tests can reveal increased amounts of protein in protein-losing enteropathy, increased amount of fat in pancreatic disease, blood in inflammatory bowel disease, etc.
Complications
Complications of protein deficiency include failure to grow, increased risk of infections, fatty liver, impaired kidney function, impaired brain function in infants, or death [100-p.609].
Treatment
Treatment of kwashiorkor and marasmus includes replacement of minerals and vitamins, carbohydrates and fats (small amounts initially) to provide calories, followed by proteins (milk-based formula for children).
Decreased Blood Albumin Levels in Inflammation
Low blood albumin levels can be caused by infection or inflammation: hepatitis, (HIV/AIDS), arteritis (vasculitis), chronic kidney disease, burns, sepsis, and also trauma or surgery.
References: [101,102,124,125,126]
Protein Supplements
Protein Supplements and Physical Performance
Conclusions of several systematic reviews of studies about the effect of protein supplements during resistance training are mixed: from no effect on endurance performance [112] or muscle function after exercise [75] to possible positive effect on muscle mass and strength, aerobic and anaerobic power in both younger and older individuals [76,107].
Protein supplements seem to have no effect on muscle mass gain in the initial weeks of resistance training in previously untrained individuals [107].
Whey Powder
Composition
- Whey concentrate can contain 35-80% protein; the rest is mostly lactose [52].
- Whey protein isolate contains 90-96% protein and, sometimes, some lactose [52].
- Whey protein hydrolysate contains parts of protein that has been broken down (hydrolyzed) to short chains of amino acids (dipeptides, tripeptides) and some free amino acids; it is absorbed faster than intact whey protein and and also less commonly triggers allergic reactions [52].
- Liquid whey and “protein water,” which is purified water with added whey, are on the market.
- Certain whey protein powder products may have vitamins or minerals added.
Whey protein contains high amount of branched-chain amino acids (BCAAs) leucine, isoleucine and valine, and other essential amino acids [52,55].
Benefits
According to European Food Safety Authority (EFSA), there is no cause-effect relationship between whey protein consumption and muscle mass gain, strength or endurance, increase of lean body mass, decrease of body fat percentage, decrease of muscle fatigue after training, satiety and weight maintenance [54]. This suggests that whey is not a better muscle weight gainer than other proteins; it is calorie intake that affects weight not the type of protein you use.
In one study in old women, adding 30 grams of whey protein and 600 mg of calcium per day did not have any beneficial or harmful effects on bone health [137].
There is insufficient evidence about beneficial effects of whey in treating HIV/AIDS [56] or reducing allergies in formula-fed infants [61].
Whey Safety: Side Effects, Dangers
Whey is possibly safe to use for most adults in single doses up to 50 grams, or 30 grams per day for 6 months [58]. According to Natural Medicines Comprehensive Database, whey may case low blood glucose levels (hypoglycemia) in individuals with diabetes mellitus and increase the risk of bleeding in individuals with bleeding disorders [58].
There are insufficient data about whey safety during pregnancy [58].
Side effects:
- In individuals with lactose intolerance, whey supplements that contain lactose can cause bloating, nausea, loss of appetite, abdominal cramps and diarrhea [59].
- Individuals with milk protein allergy can experience itching and swelling of the face, rash, nausea, vomiting and diarrhea [58].
- In one 27-year old male weightlifter, supplementation with whey for 4 weeks and creatine for 8-9 months resulted in cholestasis (bile retention in the liver) with jaundice [57].
- Other side effects may include excessive thirst, fatigue, drowsiness, sedation and headache [58].
Other Protein Supplements
- Casein is the main protein in cow’s milk and cheese [60]. Allergy to casein is possible but is less common than allergy to whey protein.
- Egg white protein
- Vegetable proteins: soy, rice and pea protein
Amino Acid Supplements
- Branched-chain amino acids (BCAAs) and other amino aids are available as tablets.
- Individuals who have severe food protein allergies, chronic pancreatitis or malabsorption disorders can get amino acid-based medical foods as a source of protein [114].
- Patients who cannot eat due to gastrointestinal disorders or need bowel rest after surgery, can get an infusion of amino acids into a vein as a source of protein [113].
Legality
Whey, casein and amino acids are not on the World Anti-Doping Agency (WADA) prohibited list [117].
NOTE: Whey and other protein supplements are not the same as the illegal anabolic androgenic steroids.
Albumin
An infusion of albumin, a type of blood protein, into a vein can be used to restore blood volume in shock or to replace lost albumin in nephrotic syndrome or burns [127].
Protein in Urine (Proteinuria)
Small amounts of protein in urine are normal. Vigorous exercise, cold or heat exposure, emotional stress and normal pregnancy can transitionally increase the amount of protein in urine. Some people have proteinuria when standing, so during the day, but not at night when lying down (orthostatic proteinuria).
Common health disorders with increased protein excretion in urine include systemic infections, urinary tract infections, kidney disorders (nephrotic syndrome with facial and feet swelling), heart disease, high blood pressure (including high blood pressure during pregnancy ─ preeclampsia or eclampsia), diabetes mellitus (excessive urination, fatigue), rheumatoid arthritis, systemic lupus erythematosus and certain cancers, lithium, lead, mercury intoxication [8].
High-protein diet does not likely increase urine protein levels in healthy individuals but can do so in those with a kidney disease.
A typical symptom of increased protein in urine is foamy urine.
Protein Interactions with Other Nutrients
Water. Each gram of protein you consume requires about 8 grams of water in order for the waste products of protein metabolism (urea) to be excreted in urine [45]. So, for every 100 grams of protein you consume, you can lose about 800 grams of water with urine. You can easily replace this loss by drinking water, so a high-protein diet by itself does not cause dehydration.
Zinc. Protein slightly increases zinc absorption [35]. Adding small amounts of animal proteins to legume meals can significantly increase zinc absorption [36].
Magnesium. Severe protein malnutrition may impair magnesium absorption [128].
Frequently Asked Questions
1. What is organic protein?
Chemically, all food proteins are organic substances. However, to be “certified organic”, a food product has to have a certificate, for example, in the US, the “USDA organic” certificate. Certified organic foods are produced without the use of artificial fertilizers, pesticides, growth stimulators, hormones or antibiotics and they do not contain synthetic colors or preservatives.
Proteins
- Fructose
- Galactose
- Glucose
- Isomaltose
- Isomaltulose
- Lactose
- Maltose
- Mannose
- Sucrose
- Tagatose
- Trehalose
- Trehalulose
- Xylose
- Erythritol
- Glycerol
- Hydrogenated starch hydrolysates (HSH)
- Inositol
- Isomalt
- Lactitol
- Maltitol
- Mannitol
- Sorbitol
- Xylitol
- Fructo-oligosaccharides (FOS)
- Galacto-oligosaccharides (GOS)
- Human milk oligosaccharides (HMO)
- Isomalto-oligosaccharides (IMO)
- Maltotriose
- Mannan oligosaccharides (MOS)
- Raffinose, stachyose, verbascose
- SOLUBLE FIBER:
- Acacia (arabic) gum
- Agar-agar
- Algin-alginate
- Arabynoxylan
- Beta-glucan
- Beta mannan
- Carageenan gum
- Carob or locust bean gum
- Fenugreek gum
- Galactomannans
- Gellan gum
- Glucomannan or konjac gum
- Guar gum
- Hemicellulose
- Inulin
- Karaya gum
- Pectin
- Polydextrose
- Psyllium husk mucilage
- Resistant starches
- Tara gum
- Tragacanth gum
- Xanthan gum
- INSOLUBLE FIBER:
- Cellulose
- Chitin and chitosan
- FATTY ACIDS
- Saturated
- Monounsaturated
- Polyunsaturated
- Short-chain fatty acids (SCFAs)
- Medium-chain fatty acids (MCFAs)
- Long-chain fatty acids (LCFAs)
- Very long-chain fatty acids (VLCFAs)
- Monoglycerides
- Diglycerides
- Triglycerides
- Vitamin A - Retinol and retinal
- Vitamin B1 - Thiamine
- Vitamin B2 - Riboflavin
- Vitamin B3 - Niacin
- Vitamin B5 - Pantothenic acid
- Vitamin B6 - Pyridoxine
- Vitamin B7 - Biotin
- Vitamin B9 - Folic acid
- Vitamin B12 - Cobalamin
- Choline
- Vitamin C - Ascorbic acid
- Vitamin D - Ergocalciferol and cholecalciferol
- Vitamin E - Tocopherol
- Vitamin K - Phylloquinone
- Curcumin
- FLAVONOIDS:
- Anthocyanidins
- Flavanols: Proanthocyanidins
- Flavanones: Hesperidin
- Flavonols: Quercetin
- Flavones: Diosmin, Luteolin
- Isoflavones: daidzein, genistein
- Caffeic acid
- Chlorogenic acid
- Lignans
- Resveratrol
- Tannins
- Tannic acid
- Alcohol chemical and physical properties
- Alcoholic beverages types (beer, wine, spirits)
- Denatured alcohol
- Alcohol absorption, metabolism, elimination
- Alcohol and body temperature
- Alcohol and the skin
- Alcohol, appetite and digestion
- Neurological effects of alcohol
- Alcohol, hormones and neurotransmitters
- Alcohol and pain
- Alcohol, blood pressure, heart disease and stroke
- Women, pregnancy, children and alcohol
- Alcohol tolerance
- Alcohol, blood glucose and diabetes
- Alcohol intolerance, allergy and headache
- Alcohol and psychological disorders
- Alcohol and vitamin, mineral and protein deficiency
- Alcohol-drug interactions